Introduction: Specialty clinics during the core medicine clerkship pose particular challenges for medical students, who often lack the specialized knowledge to fully engage in the clinic and may be pushed into an observational role, which undermines self-efficacy. 1 Self-efficacy theory focuses on the impact self-perceived capability has on achieving educational outcomes. A dissatisfying experience may also limit students' interest in pursuing a career in clinic-based subspecialties such as non-malignant hematology. Given the projected deficit of hematology providers and evidence that a large proportion of those who elect to become hematologists develop their interest during medical school, 2,3 this represents a serious consequence. We sought to improve the hematology student clinic experience to better serve education and engender a long-term interest in hematology by focusing on self-efficacy.
Methods: We developed a flipped classroom model to allow students to prepare the hematologic content of clinic visits prior to arrival and then focus their time in clinic on executing visits. All core clerkship students rotating through hematology clinic were eligible to participate in the study. Participating students were pre-assigned two patients with a review article for each visit and completed surveys pre- and post-clinic. Surveys items covered self-efficacy 4 and interest in hematology on a five point Likert scale. Distributions for each survey item were compared pre- and post-clinic and tested for statistical significance with Chi-square tests.
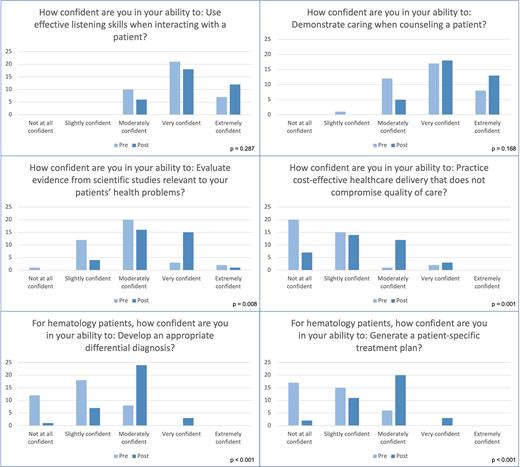
Results: During the two years from May 2021 through April 2023, 103 students rotated through hematology clinic with 38 students (37%) opting to participate in the study. Two of the 38 students did not complete the post-clinic survey. Students had a statistically significant increase in four of six measures of self-efficacy (See Figure). Students reported increased self-efficacy in evaluation of research relevant to patient care and practicing cost-effective care (p = 0.008 and 0.001, respectively). Specific to hematology, there was an increase in self-efficacy regarding creation of a differential and a treatment plan (both p < 0.001). There was no statistically significant change in self-report of effective listening or demonstration of caring, which were also the two measures with the highest pre-clinic self-efficacy. While student responses were consistent with interest in more exposure to hematology or a possible career in hematology or internal medicine, this was not changed post-clinic. When comparing their experience to other clinics, 75% and 71% students rated hematology clinic slightly or much better than other medicine clinics and non-medicine clinics, respectively.
Conclusions: A structured approach to hematology clinic with pre-assigned patients and tailored preparatory reading improved self-efficacy both specific to hematology and more generally. Students rated the experience more highly than other clinics. There was no impact on career interest in hematology or internal medicine.
References
1. Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review 1977;84(2):191-215.
2. Sharma D, Wallace N, Levinsohn EA, et al. Trends and factors affecting the US adult hematology workforce: a mixed methods study. Blood Adv 2019;3(22):3550-61.
3. Hoots WK, Abkowitz JL, Coller BS, DiMichele DM. Planning for the future workforce in hematology research. Blood 2015;125(18):2745-52.
4. Artino AR, Dong T, DeZee KJ, et al. Development and initial validation of a survey to assess students' self-efficacy in medical school. Mil Med 2012;177(9 Suppl):31-7.
Disclosures
Langer:Agios: Honoraria, Speakers Bureau. Parnes:Vertex Pharmaceuticals: Current Employment.